July 25 2025 | Medication Errors: Costly Risks Worth Preventing
The frequency of medication errors resulting in resident harm is and has historically been low; insurance claims related to medication errors represent less than 2% of total claims. The potential for medication errors to cause significant harm to residents, however, has resulted in insurance claims with high severity. The average total incurred claim cost was just over $306,000 in 2024.
Medication errors are considered the administration of the wrong medication, wrong dose, wrong resident, wrong route, wrong time, or incorrect preparation. In 2024, 44% of medication errors where claims were filed against the facility involved administration of medications to the wrong resident. Incorrect medication dose accounted for 24% of medication errors resulting in claims.
The medication categories involved in medication errors with the biggest claims included opioids (44%), antiepileptic (8%), hyperglycemic agents (8%) with the remaining 40% categorized as “other.” Of the categories, the highest claims went to errors relating to hyperglycemic agents at just shy of $427,000 per claim.
Fortunately, there are risk management recommendations that can mitigate resident harm and associated costly claims. Creating, implementing, and monitoring robust medication systems ensure medications are dispensed, prepared, and administered correctly. Standardizing procedures and collaborating on a culture of safety can improve resident outcomes and minimize medication errors. The following suggestions can enhance safety with medication management:
RESIDENT IDENTIFICATION AND DOSE VERIFICATION. Consider at least two resident identifiers (for example, asking them their name and date of birth, and confirming with a current photo) before administering or assisting with medications. For high-risk medications, implement a double verification process to confirm the accurate dose was prepared. Implement a barcode scanning system to ensure the correct medication is given at the right dose and time for the right resident.
MEDICATION RECONCILIATION. Regularly review and update residents’ medication lists to minimize errors related to outdated information. Reconcile medications upon admission/move-in, transfer, and discharge.
STAFF EDUCATION AND ONGOING TRAINING. Provide comprehensive staff training for all staff involved in medication management. Include review and confirmation of consistent use of the facility’s procedures. Offer ongoing education and routine, proactive competency assessments to reinforce safe medication management practices.
STANDARDIZE PROCEDURES. Develop and implement standard procedures for medication assistance and administration, including double-checking protocols for high-risk medications. This is especially important with residents who have similar names. Monitor to ensure procedures are consistently followed and regularly evaluated for effectiveness, update procedures as necessary.
COMMUNICATION. Encourage staff communication regarding medication orders, changes, and concerns. Use standardized communication tools that capture critical information in a documentation format, such as SBAR (Situation, Background, Assessment/Appearance, Recommendation).
TECHNOLOGY. Implement and consistently use electronic health records that have built-in medication alerts and reminders. Use electronic medication records to document medication administration, refusals, follow-ups, and outliers. Utilize the built-in audit features to discover misses and near-misses and educate the team on findings.
ENVIRONMENTAL FACTORS. Staff who are managing medications should have limited distractions and interruptions when preparing, delivering, and documenting medications. Create a quiet, focused, nonchaotic and organized environment. Ensure medication storage is clean and clearly labeled for easy storage and retrieval. Minimize access to or use of personal electronic devices such as cell phones while conducting a medication pass.
QUALITY IMPROVEMENT INITIATIVES. Conduct regular audits and reviews of medication management processes and identify areas of improvement. Establish a system for monitoring medication passes and provide feedback to staff on findings and ways to improve. Encourage reporting and analysis of medication errors and near misses to identify root causes and implement systems to minimize recurrence.
COLLABORATION WITH PHARMACY. Involve your long-term care pharmacy partners in medication reconciliation, orders review, and monitoring for medication interactions. Engage the pharmacist’s input for best practices in handling high-risk medications or complex medication regimens.
INCIDENT REPORTING. Ensure all medication errors, including near misses, are captured via documented incident report and investigation processes. Promote a culture of safety where staff feel comfortable reporting errors and near misses without fear.
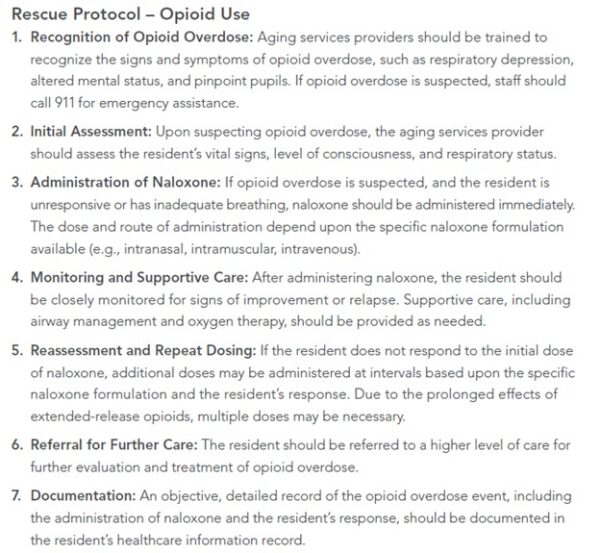
Because one of the highest-risk medication classes is opioids, the facility should develop and implement a strong rescue protocol that prompts staff to detect and immediately intervene in overdoses and adverse reactions.
Rescue protocols improve communication among staff and are essential for coordinating effective response efforts. Rescue protocols should outline individual roles; this reduces confusion during an urgent event.
Consider the following vital elements of an effective rescue protocol, and ensure your facility’s systems include the following, at a minimum (from the 2024 edition of Aging Services Claim Report):
WHCA will continue next month with this series on risk management. August’s focus will be on resident elopement. For more information on this series please email Elena Madrid (for skilled nursing providers) or Vicki McNealley (for assisted living providers).

